Massachusetts Health Connector
Strategic Plan 2024–2028
Introduction
The Massachusetts Health Connector is the country’s first and longest-running state-based health insurance Marketplace, created in 2006 as part of Massachusetts state health reform (Chapter 58 of the Acts of 2006) to provide high-value coverage to individuals and small businesses in the Commonwealth and to serve as a policy and outreach hub for both state and federal health reforms designed to expand and improve health coverage.
More than seventeen years after the organization’s inception, and ten years after Massachusetts’s implementation of the Affordable Care Act (ACA), the Health Connector continues to lead the nation in its work keeping Massachusetts residents covered at a near-universal insurance rate and through innovative actions that maximize access to affordable, comprehensive, and equitable health care. This work helps ensure that residents of the Commonwealth have the opportunity to attain the highest levels of health and are protected by the critical financial safeguards enabled by meaningful health coverage.
Residents of the Commonwealth are at the core of the Health Connector’s mission, and providing low- and moderate-income individuals, families, and small employers with access to comprehensive health coverage has remained its beacon. The 2024–2028 Strategic Plan is intended to serve as a road map for the Health Connector, providing a framework to organize agency initiatives, infrastructure, policies, and practices to ensure continued success and maximum public impact. This strategic plan is intended to allow the Health Connector to respond to and meet the moment while keeping its core mission as its North Star.
The Health Connector’s Beginnings and Growth
While the Health Connector’s mission to provide health insurance to state residents and small businesses has not changed, the organization has had to evolve significantly throughout the course of its eighteen-year history in response to a dynamic health care, policy, and business landscape. Throughout periods of change, the Health Connector continued its focus on system stability, growing enrollment among eligible residents, and enhancing its member experience, adjusting course to ensure Massachusetts residents could continue to rely on Health Connector coverage and that the Commonwealth stayed true to its goals around expanding health coverage access to all residents.
Moving forward, the Health Connector will continue to draw from its greatest assets to fulfill its mission and vision: its dedicated and passionate staff, the support of its committed Board of Directors and local, state, and national leaders, collaborative relationships with state sister agencies, and partners across the health care system and in the community. The Health Connector also enjoys strong relationships with its state partners at the Division of Insurance (which regulates the Commonwealth’s commercial “merged market” in which Health Connector coverage is situated) and the state’s Medicaid program, MassHealth, with which the Health Connector shares an integrated eligibility and enrollment system, and with which many Health Connector enrollees and/or their family members move back and forth between for health coverage. The Health Connector’s current and future successes would not be possible without the support and expertise of the diverse constituencies that played a role in pressing for the advancement of the Health Connector’s mission and the aims of state and federal health reform. Nevertheless, there is still immense work to be done to ensure equitable access to affordable, comprehensive health insurance coverage for all people and communities in the Commonwealth and that the services and coverage experience provided by the Health Connector are truly “best in class.” It is with determination, gratitude, and appreciation that the Health Connector carries the torch into this next phase of its work to serve the Massachusetts public.
Looking Forward
Looking ahead to the next five years, the Health Connector will ensure the objectives and initiatives outlined in this strategic plan continue to advance its core mission and vision and are guided by its values.
Mission Statement
Advance access to high-quality health care by serving as a transparent and transformative health insurance Marketplace for Massachusetts residents and small businesses to come together and easily find, compare, and enroll in affordable health coverage.
Vision Statement
Serve as the leading state-based health insurance Marketplace in the nation by upholding the Commonwealth’s near universal health coverage rate and making it as easy as possible for all residents to enroll in and maintain high-value health insurance coverage.
Values Guiding the Health Connector
- Person-centeredness: The real lives of residents of the Commonwealth who rely on Health Connector coverage or are touched by its policies, and how their needs differ based on lived experience, will remain at the center of all program design, policy-making, and operational decisions.
- Equity: Health Connector practices and policies will advance equitable access to comprehensive health coverage and health coverage that promotes equitable health outcomes.
- Value: Health Connector coverage will provide members with meaningful access to health services with minimal barriers due to cost, while centering the importance of an economically sustainable health care system and being good stewards of public (state and federal) resources.
- Reliability: The Health Connector will serve as a reliable and trustworthy source of coverage to the residents it serves, and as a dependable and steady business and policy partner to its stakeholders.
The Health Connector’s 2024–2028 Strategic Plan was developed based on staff, management, and the Board of Directors’ careful reflections on the Health Connector’s work to date and opportunities for heightened impact in the years ahead. It also incorporates feedback solicited from a diverse set of external stakeholders, including Board Members, carriers, navigator organizations, legislative and congressional offices, health care advocates, employers and health insurance brokers, and state and partner agencies via surveys assessing the Health Connector’s successes, challenges, and opportunities moving forward.
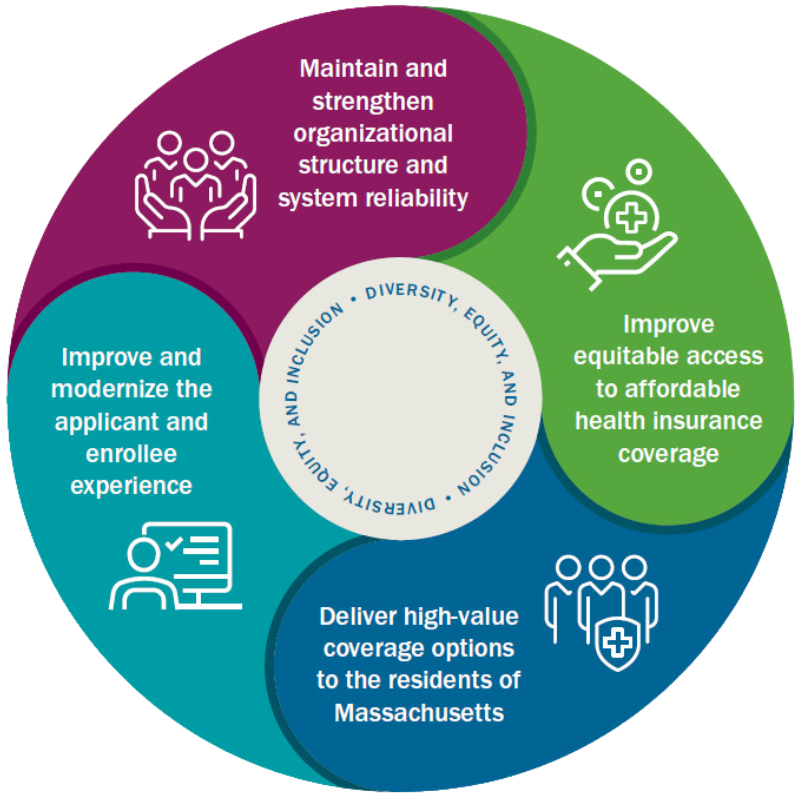
This strategic plan outlines eight broad goals and associated initiatives that fit within four overarching focus areas identified through the planning process:
- Improve and modernize the applicant and enrollee experience
- Maintain and strengthen organizational structure and system reliability
- Improve equitable access to affordable health insurance coverage
- Deliver high-value coverage options to the residents of Massachusetts
A Commitment to Using the Health Connector as a Tool for Promoting Equity
The Health Connector recognizes that both state and federal health reform and the creation of the Health Connector were direct policy responses on behalf of the Massachusetts and American public to an inequitable health coverage landscape that left key populations (e.g., Black and Hispanic populations, immigrant groups, those who don’t speak English as a first language, lower-income individuals, people with health issues, LGBTQ+ people, workers without employer-based coverage, and small employers) out of the health and economic protections afforded by health coverage. The Health Connector, therefore, understands itself to be explicitly charged with using the policy, program, and business tools at its disposal to name and counter these structural problems as they are encountered in its work. The Health Connector will continue to act with intention as it centers racial equity and other forms of equity into existing program and policy work it does in the public interest, as well as future initiatives spurred by this strategic plan. Further, the Health Connector recognizes that equity in the context of health insurance is a distinct (and underexplored) dimension of the equity agenda that it aims to more deeply articulate and act upon.
The Health Connector also recognizes the importance of championing diversity, equity, and inclusion throughout the Health Connector’s internal day-to-day operations, in addition to its service to the public and the work that will be animated by this strategic plan.
Adoption and Use of 2024–2028 Strategic Plan
The 2024–2028 Health Connector Strategic Plan will serve as a set of guideposts for the work of the Health Connector and its staff over the next five years. Outlining a common vision towards which the agency can advance, the strategic plan is also intended to (1) strengthen the foundation of the Health Connector to be adaptable and agile, and (2) better prepare the organization to respond to opportunities to advance its mission and surmount potential obstacles on the road ahead.
Annually, the Health Connector will establish and align its focus and priorities for the coming year with the goals outlined in the strategic plan. The yearly process will allow the Health Connector to remain responsive to changing dynamics, intentionally identifying its tactical approach, and precise in quantifying its expected achievements and progress measurements. The strategic plan document will be regularly used to assess the direction of existing and future agency initiatives to ensure that they align with agency priorities and goals articulated in the strategic plan.
Areas of Strategic Focus, Goals, and Initiatives
Improve and modernize the applicant and enrollee experience
Modernize and streamline the experience of applicants and enrollees to ensure that they can obtain and maintain health insurance coverage with ease. Individuals should be able to easily and independently navigate and access Health Connector tools and resources, with minimized administrative burdens or bureaucratic obstacles.
1. Ensure residents can seamlessly and quickly enroll in and easily maintain coverage
2. Provide a more user-friendly, streamlined online experience for residents and members engaging digitally with the Health Connector
Measuring Outcomes
Maintain and strengthen organizational structure and system reliability
Ensure Health Connector staff and systems can adapt and grow to reliably meet the needs of state residents and an ever-evolving health coverage, technology, and business landscape.
1. Foster an inclusive work environment that centers professional growth and staff empowerment
2. Ensure, invest in, and cultivate reliable Health Connector organizational functions
Measuring Outcomes
Improve equitable access to affordable health insurance coverage
Use available policy, operational, and communication tools to reduce and remove barriers that prevent access to affordable health insurance coverage for all Massachusetts residents.
1. Expand equitable access to affordable health coverage
2. Evaluate and address health equity initiatives through data analytics and community engagement
Measuring Outcomes
Deliver high-value coverage options to the residents of Massachusetts
Enhance affordability for members and those within the merged market (the state’s combined individual and small group insurance markets) more broadly, ensuring that members can use their coverage to access health care services that enable them to attain their highest level of health and financial stability.
1. Ensure Health Connector coverage is comprehensive, affordable, and meets residents’ needs
2. Increase awareness of the value and brand of Health Connector products
Measuring Outcomes
Conclusion
The Health Connector looks forward to advancing this next phase of its work delivering the health care access and financial protections afforded by comprehensive health coverage to the Massachusetts public and serving as the nation’s leading state-based health insurance Marketplace. Health Connector leadership and staff will work with its Board of Directors, MassHealth leadership, and external stakeholder partners to be guided by the principles and guideposts outlined in this strategic plan and by the mission of the agency and its focus on promoting and improving access to high-value, affordable health insurance coverage.
Health Connector leadership and staff will provide updates to its Board of Directors and the public on the progress made in advancing the goals and objectives outlined in the strategic plan and looks forward to continuing to challenge itself and hold itself accountable to further expanding and strengthening its impact in the Massachusetts health coverage landscape.






