Throughout the year your circumstances may change which may make you eligible for a Special Enrollment Period (SEP). If you have a baby, you or your dependent gain or lose other coverage, etc., you may be able to change your plan, enroll in a plan for the first time, add or drop family members, or terminate your plan. You must report the event WITHIN 30 DAYS of the event to be eligible for an SEP. Once you report the event in your account, DC Health Link will guide you through the options available to you and your family.
Step 1: Report the Qualifying Life Event
In each employee’s account, consumers will have the option to report a qualifying life event. Please select the life event that applies to the primary subscriber or dependent (For Example: “Drop coverage due to new eligibility”).
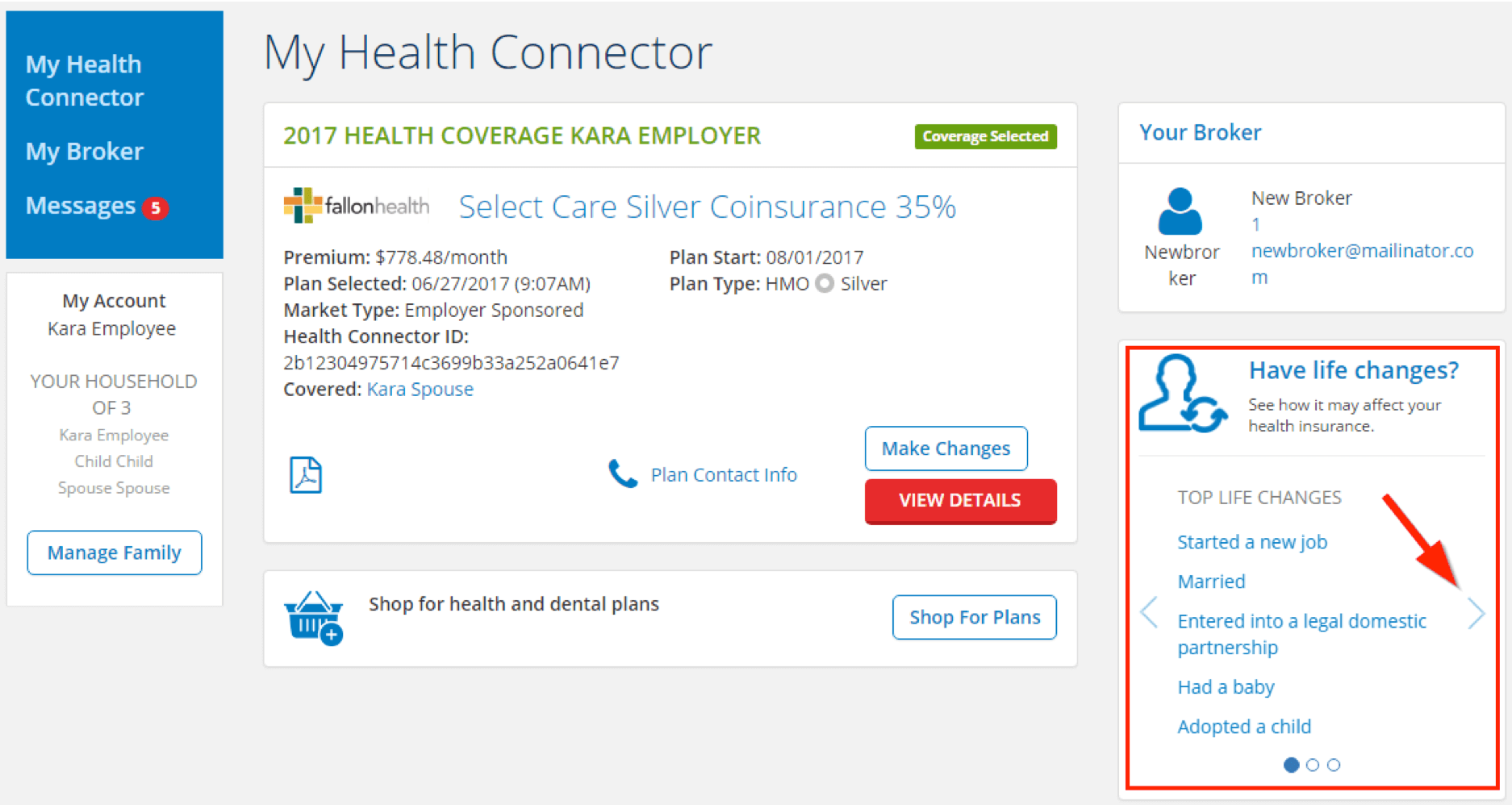
Note: There are three different pages of QLEs that can be viewed by clicking the arrow
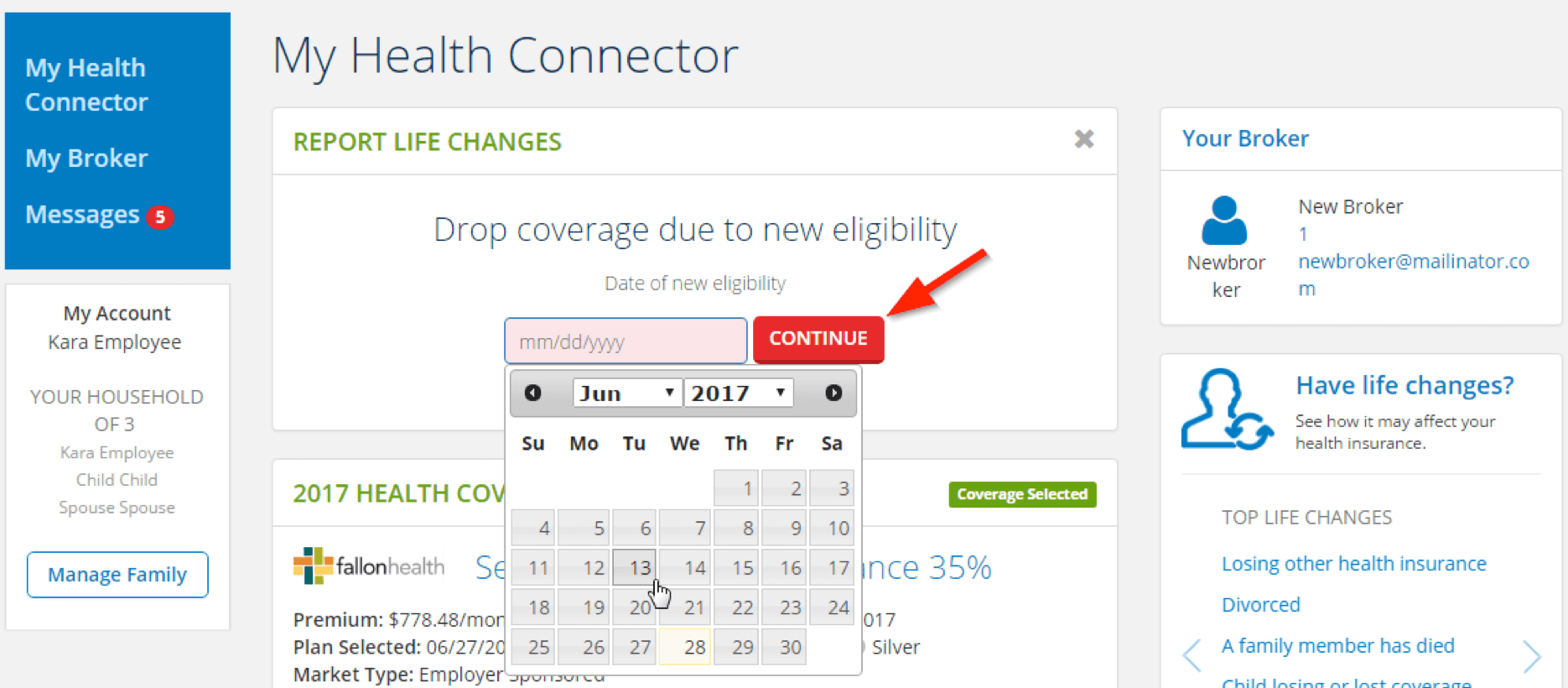
Step 2: Enter the Date of QLE
Report the date of your qualifying event by selecting the date from the calendar or keying in the date. Then click “Continue”.
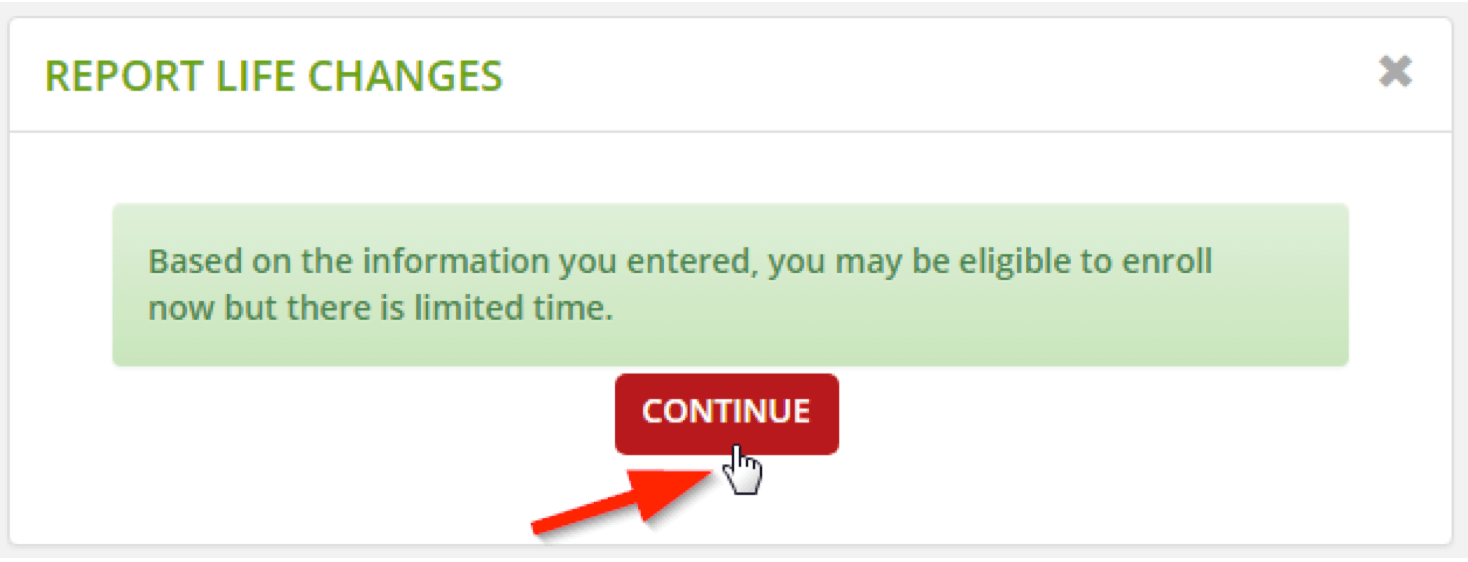
Step 3: Confirm the QLE
If you are eligible to apply for a SEP, a green confirmation box will appear. Click “Continue” to proceed.
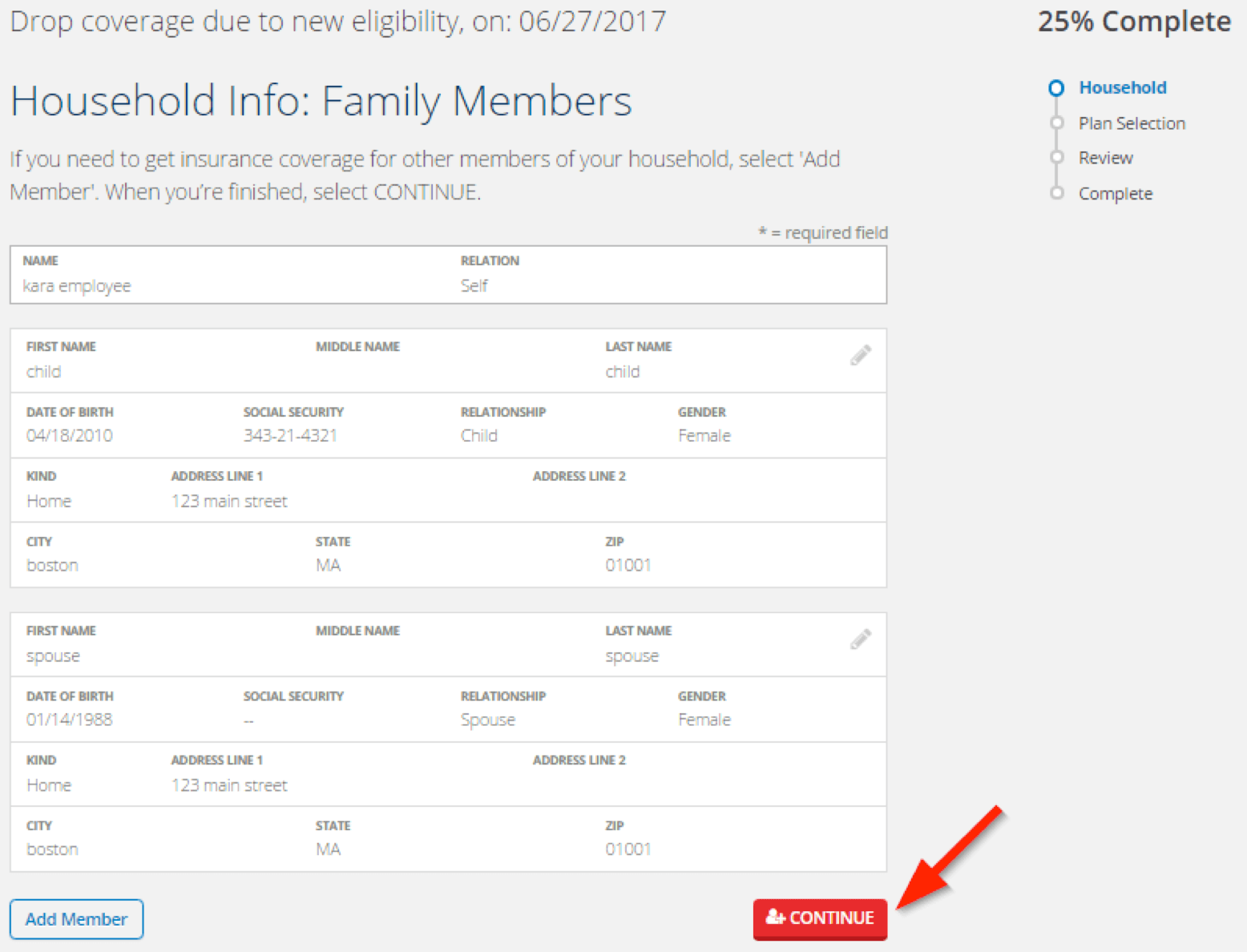
Step 4: Confirm Household
Once you have confirmed your household, click the “Continue” button.
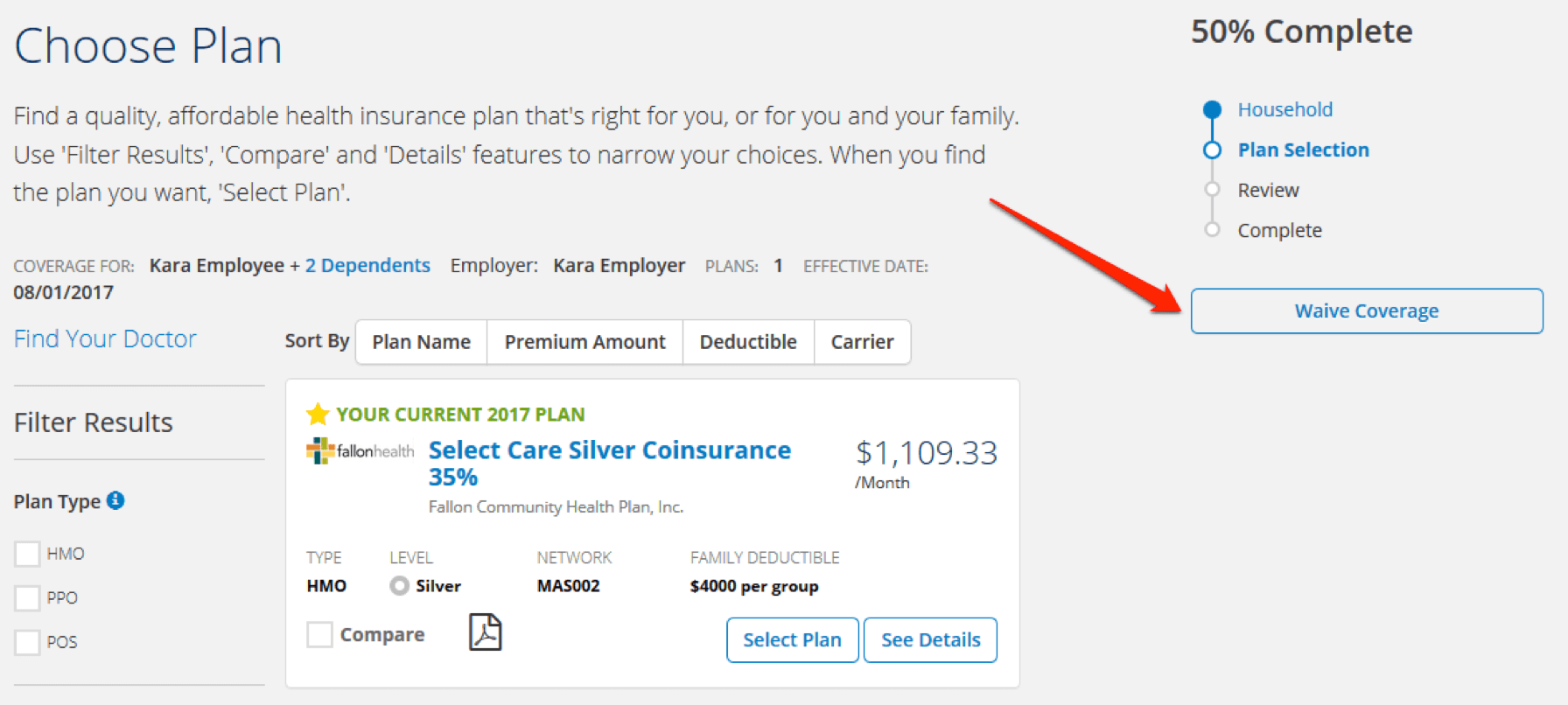
Step 5: Select Waive Coverage
Click “Waive Coverage” for the plan that you wish to terminate.
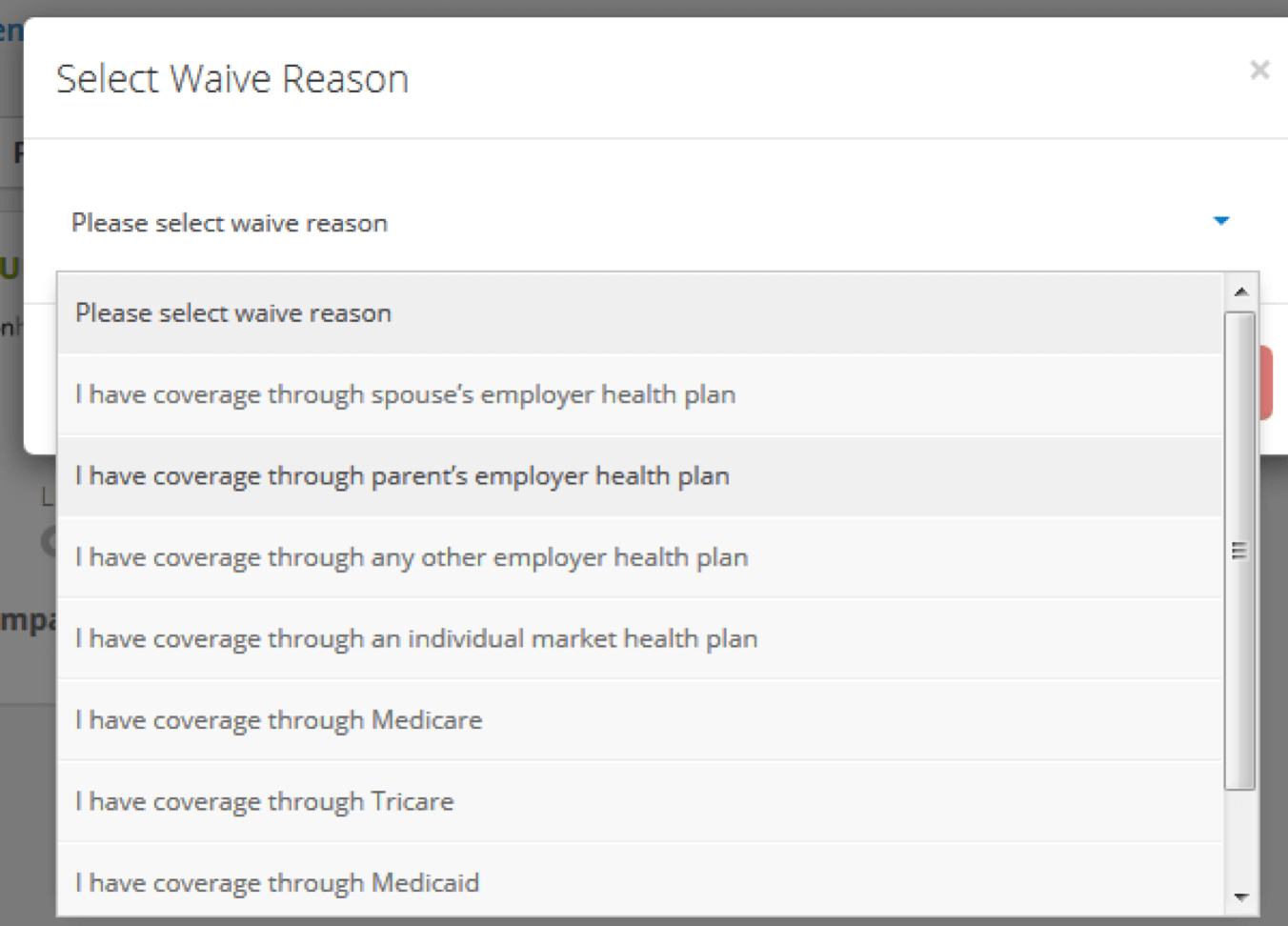
Step 6: Select Waiver Reason
Select the reason why you are waiving coverage.
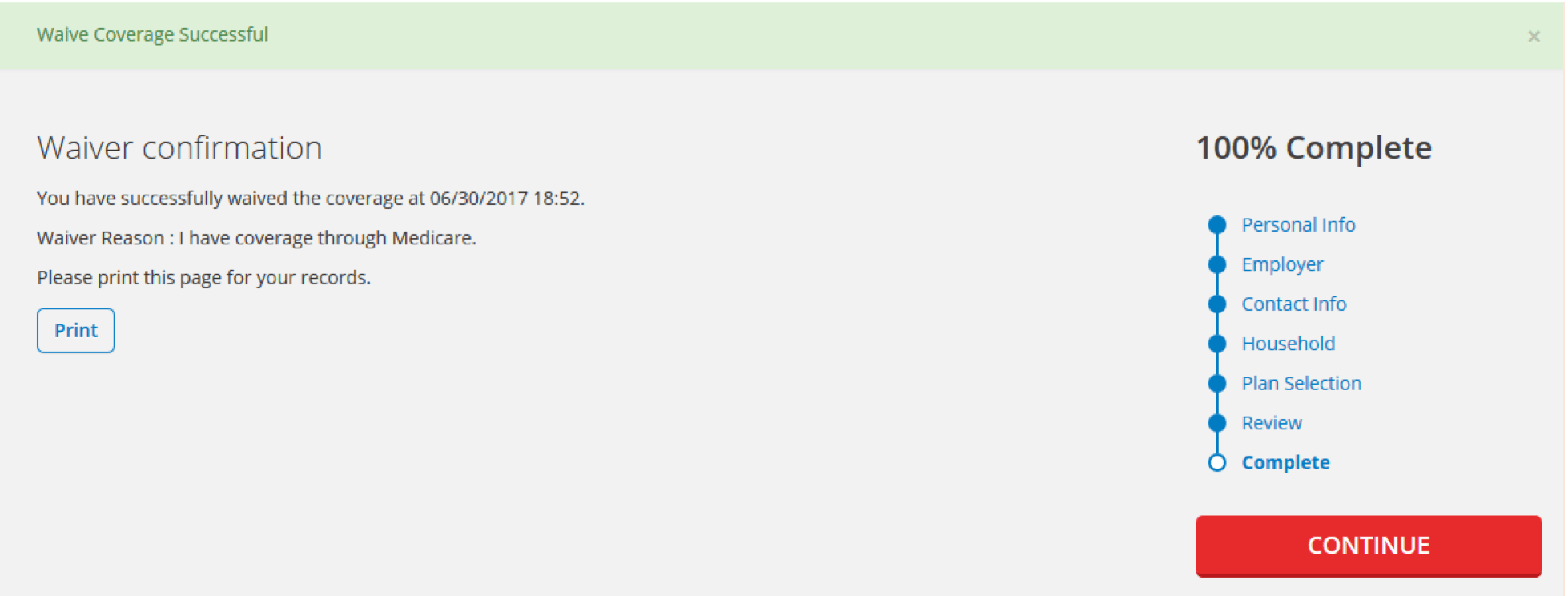
Step 7: Waiver Confirmation
You will see a green “Waive Coverage Successful” banner. You can either print this page or continue to your account homepage.