Health Connector Walk-In Centers Are Closing in 2025
The Springfield walk-in center closed on March 28, 2025. Worcester and Boston locations remain open until May 23 and June 27, respectively.
Find out more about these closures →
Getting Started Guide
The Commonwealth is dedicated to ensuring people who apply for coverage and shop for plans on the website have the best experience possible. Below, please find important information to know before you get started, as well as tips and clarifications about the online application. Check back often for updates.
Top Questions and Answers:
General Information
If you need health coverage now, there’s good news! You can enroll in health coverage any time of the year if you experience a qualifying event or are newly eligible for help paying for health coverage. Programs include MassHealth, Children’s Medical Security Plan (CMSP), Health Safety Net, and ConnectorCare. Find out more →
Monthly Plan Selection and Payment Deadlines
| Payment Due Date | Coverage Start Date |
|---|---|
| December 23, 2024 | January 1, 2025 |
| January 23, 2025 | February 1, 2025 |
| February 23, 2025 | March 1, 2025 |
| March 23, 2025 | April 1, 2025 |
| April 23, 2025 | May 1, 2025 |
| May 23, 2025 | June 1, 2025 |
| June 23, 2025 | July 1, 2025 |
| July 23, 2025 | August 1, 2025 |
| August 23, 2025 | September 1, 2025 |
| September 23, 2025 | October 1, 2025 |
| October 23, 2025 | November 1, 2025 |
| November 23, 2025 | December 1, 2025 |
| December 23, 2025 | January 1, 2026 |
It will be helpful to have some of this information ready to look at as you fill out your application. Also, you may be asked to send us copies of some of these documents or others if we need more proof from you after we get your application.
- Social Security numbers for all people who are applying (if they have one).
- Immigration documents for all non-U.S. citizens who are applying (if they have one). Find more information about immigration documents.
- A copy of your federal tax return from last year. If you did not file taxes last year, or your income has changed since last year, have information about your current income ready (such as recent pay stubs or an unemployment award letter).
- Home address or mailing address (if applicable) for everyone in your household who needs insurance, unless they are homeless.
- If you are found eligible for coverage through the Health Connector and you plan to make a payment online, you will need your banking institution routing number and account number for either your checking or savings account (if you have a premium).
- If you are found eligible for coverage through the Health Connector and you plan to make a payment by mail or in-person, you will need a personal check or money order to make a payment for your first month’s premium (if you have one).
- If your employer offers health insurance, ask your employer these questions:
- Do any of the health plans that the employer offers meet the “minimum value” standard?
- What is the employee contribution to the lowest-cost health plan offered by your employer for an individual?
- How often?
- Weekly
- Every 2 weeks
- Twice a month
- Monthly
- How often?
Your eligibility determination depends upon your household size, income, and other factors that you will provide during the application process. When applying for coverage, tell us about all the household members who live with you. If you file taxes, we need to know about everyone on your tax return. You do not need to file taxes to get MassHealth, the Health Safety Net, or the Children’s Medical Security Plan, if you qualify.
DO include
- Yourself and your spouse (if married)
- Your natural, adoptive, or step children younger than age 19
- Your unmarried partner who lives with you if you have children together who are younger than age 19
- Your unmarried partner’s children who live with you and who are younger than age 19, if you also include this partner
- Anyone you include on your tax return (even if they do not live with you)
- Anyone your unmarried partner included on his or her tax return (even if they do not live with you), if you also include your unmarried partner
- Anyone else younger than age 19 who you live with and take care of
DO NOT include
- Your unmarried partner, unless you have children together
- Your unmarried partner’s children, unless they live with you or your unmarried partner included them on his or her tax return
- Your parents whom you live with if your parents file their own taxes and do not claim you as tax dependent (if you are age 19 or older)
- Other adult relatives whom you do not claim as tax dependents
The amount of help or type of program you may qualify for depends on the number of people in your household and their incomes. This information helps us make sure everyone gets the coverage they may be eligible for. Complete the required application information for yourself and all additional household members who live with you, or anyone on your same federal income tax return if you file one. If you do not file a tax return, remember to still add household members who live with you.
In order to protect your privacy, the Health Connector has some built-in features to keep your information private and protected. But, there are also actions you can take to keep your information secure:
- Never leave your computer or mobile device unattended during your session. It’s easy to protect your information by logging out of your account when you are finished with each session. To ensure cached copies of your pages are cleared, always close your browser—not just the tab you are working in—after logging out.
- Your website session will expire after 20 minutes of inactivity. If you are still working on your application, but stepped away from the computer for 20 minutes or more, you may lose unsaved information. To continue working, you will need to log back into the site.
- If your browser offers to save your username or password, always choose “No” to prevent other people who may use the computer to access your account.
- Do not leave your username or password written down where another person may find it.
Always close your browser—not just the tabs in your web browser—when you are finished using the Health Connector website, especially if you are using a public computer.
No. If you already have an account, you must not create a new one. If you are locked out of your account, or forgot your username or password, see the section on MA Login, below, to help troubleshoot.
Technical Issues and Troubleshooting
If you use an older web browser that does not support the online application, such as Internet Explorer (IE) 11 or older, some functions may not work as they are supposed to and can result in difficulties when browsing the site or completing your application. You should upgrade your current browser to the latest version.
If you experience technical issues while using this website, many can be resolved by clearing your browser’s memory (also called “cache”). Below are instructions on how to do this in the recommended web browsers:
Chrome version 30 or later
- Click the Chrome menu button (three horizontal bars in the top right corner on the browser toolbar, or three dots).
- Select “Tools.”
- Select “Clear browsing data.”
- In the dialog that appears, select “Empty the cache” and deselect other items.
- Use the menu at the top to select the amount of data that you want to delete. Select “beginning of time” to delete everything.
- Click “Clear browsing data.”
Get more detailed instructions on how to clear your cache in Google Chrome
Firefox version 30 or later
- Select “History,” and select “Clear Recent History.”
- For the “Time range to clear” section, select “Everything.”
- Click on the dropdown for the “Details” menu and check the box “Cache.”
- Click “Clear Now.”
Get more detailed instructions on how to clear your cache in Mozilla Firefox
Microsoft Edge
- Select Settings and more > Settings > Privacy, search, and services .
- Under Clear browsing data, select Choose what to clear.
- Choose a time range from the Time range drop-down menu.
- Choose the types of data you want to clear (see the table below for descriptions). For example, you may want to remove browsing history and cookies but keep passwords and form fill data.
- Select Clear now.
Get more detailed instructions on how to clear your cache in Edge
The Health Connector website uses strong web security settings. If you use are using an older web browser, you may need to update your web browser’s security settings in order to use the Health Connector website. See below to learn how you can make sure you have the correct browser security settings in order to use the website:
Internet Explorer Browsers
- Open Internet Explorer
- From the menu bar, click Tools > Internet Options > Advanced tab
- Scroll down to Security category, check the option box for Use TLS 1.1 and Use TLS 1.2
- Click OK
- Close your browser and restart Internet Explorer
Chrome Browsers
- Update to the latest version browser.
Firefox Browsers
- Update to the latest version browser.
Chrome version 30 or later
- Click the Chrome menu button (three horizontal bars in the top right corner on the browser toolbar).
- Select “Tools.”
- Select “Clear browsing data.”
- In the dialog that appears, select “Empty the cache” and deselect other items.
- Use the menu at the top to select the amount of data that you want to delete. Select “beginning of time” to delete everything.
- Click “Clear browsing data.”
Get more detailed instructions on how to clear your cache in Google Chrome
Firefox version 30 or later
- Select “History,” and select “Clear Recent History.”
- For the “Time range to clear” section, select “Everything.”
- Click on the dropdown for the “Details” menu and check the box “Cache.”
- Click “Clear Now.”
Get more detailed instructions on how to clear your cache in Mozilla Firefox
Internet Explorer 11
- Select “Tools,” and select” Internet Options.”
- Under “Browsing History,” select “Delete.”
- Check the following: “Temporary Internet Files, Cookies and History.”
- Select “Delete.”
- Click “OK” to close Internet Options dialog box.
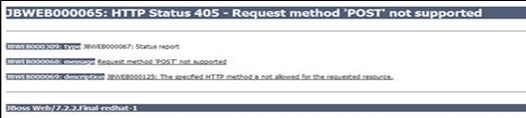
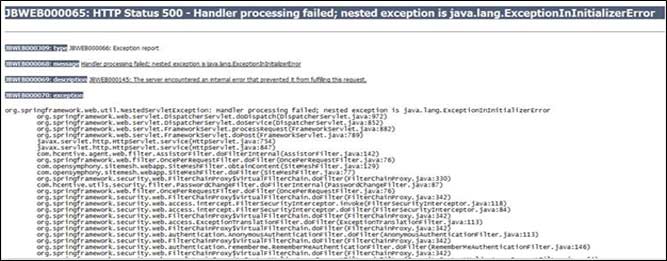
If you have tried these things and are still getting 405, 500, or general error message (see example images below), you can come back to the site and try again later. If you continue to experience these errors, you can also call customer service at 1-877-MA-ENROLL (1-877-623-6765), or TTY 711 for people who are deaf, hard of hearing, or speech disabled.
Example 405 Error:
Example 500 Error:
General Error Message Page:

Applying for Coverage
You do not have to complete your application all at once. The application is separated into different sections. Each section has an introduction page that explains:
- What the section is about,
- What you will need to complete the section, and
- An estimated time to complete that section.
If you do not think you will have the time to complete the application in one sitting, you can always save your application at the end of a section and come back later to complete it. Please review the Important Dates and Deadlines section so you know when you need to act.
Before you apply for coverage, did you know you can preview plans available in your area? To get started, go to the Get an Estimate tool.
Remember, because this is anonymous, none of your information will be saved.
Please note that the premiums shown are just estimates. You will need to complete an application to see if you qualify for help paying for costs to see your actual rates.
How to Create an MA Login
Go to the application and click the Apply Now button to start creating your account.
Step 1:
- First Name – Enter your first name. It is a mandatory field.
- Last Name – Enter your last name. It is a mandatory field.
- Year of Birth – Enter your year of birth in YYYY format. For example, 1990. It is a mandatory field.
- Email Address – Enter your email address. It is a mandatory field
- MA Login – Enter your preferred ID. It is a mandatory field.
Create your MA Login by using the following guidelines:
-
- Enter a minimum of 6 characters and maximum 50 characters.
-
- Use at least one letter.
-
- Do not use spaces.
-
- Do not use letters with accents.
-
- Do not use the following symbols: % + ” & [ ] ^ ‘ { | } < > # , / ; ( ) : * = ~
- Password – Enter your password for the application. It is a mandatory field.
- Confirm Password – Enter your password again. It is a mandatory field.
- Phone Number – Enter your phone number along with your country code. For example, +1 XXX-XXX-XXXX.
Step 2:
- Select the Terms of Use and Website Privacy Policy links to read and accept the conditions.
Step 3:
- Select Continue to receive the email with activation code and link to verify your email address.

Step 4:
- Go to your mailbox and open the email with the activation code and link for your MA Login.

Step 5:
- Select Verify my MA Login to complete your email verification.
OR
- You may copy the activation code from your email and paste it in the Enter Activation Code field on the Verify Your Email Address page.
- Select Verify.

Step 6:
- Select either Text Message or Call Me option on the Verify Phone Number Page to receive the Access code for phone verification.

Step 7:
- Enter the Access code on Verify Phone Number page and select Verify to complete the phone verification.
- The system completes the validation of your email address and phone number and displays the following success message “Email Address & Phone number are verified Your MA Login is ready to use”
If you don’t remember your login information, you can reset your username or password.
If you forget your username or password, you can go to the account sign in page and click on the link “Forgot Username” or “Forgot Password” to get an email from MA Login that will include information and instructions to get back into your account.
Please note that these emails will come from MA Login. If you do not get an email within a few minutes, check your email’s spam or junk email folder. If this happens, please add the MA Login to your safe-senders list.
Please note: The only required information for this form is your first name and your last name.
I am locked out of my MA Login account. What should I do?
First, follow the instructions above to reset your username or password. If you are not able to get back into your account by clicking the “Forgot username” or “Forgot Password” links (see above), you can call Health Connector customer service for help at 1-877-MA-ENROLL (1-877-623-6765), or TTY 711 for people who are deaf, hard of hearing, or speech disabled.
When I try to sign in, I get a message that there is already an MA Login account
If you get a message that there is already an account created with your login information, you may need to go through the “I forgot my account username and/or password” process as described above. If you continue to get this message, you can call Health Connector customer service for help at 1-877-MA-ENROLL (1-877-623-6765), or TTY 711 for people who are deaf, hard of hearing, or speech disabled.
If you are still having login issues
- Try closing and restarting your web browser. This may resolve your login issues.
- Clear your browser’s cache (read the information in the section above to learn how to do this).
If you are applying for coverage with the help of an Enrollment Assister, family member, or friend, there is a section of the application that allows you to indicate if someone is helping you. You will need to select “Yes” or “No” before you can continue.
Please note that you are not required to have someone help you in order to apply or receive benefits.
If you are applying with help from another person, when you select “Yes,” you will also need to provide information about that person on that screen. If you are getting help, you will need to provide the required information on the “Who is helping you” screen during the application before you can continue your application.
For some of the types of people that help you, like a Navigator or Certified Application Counselor (CAC), you will also be asked to fill out a form that gives them permission to help you:
| Enrollment Assister Type | Form(s) to Complete |
| Navigator | Navigator Designation Form (NDF) |
| Certified Application Counselor | Certified Application Counselor Designation Form (NDF)and sometimes also a Permission to Share Information (PSI) Form |
| Issuer Enrollment Assister | Issuer Enrollment Assister Designation Form |
When you meet with an Enrollment Assister, they will provide you with the form to complete.
Who can help me?
You can get help from a friend, family member, relative, or other person or organization of your choosing who agrees to help you. Or, you can get help for a certified Enrollment Assister such as a Navigator, Certified Application Counselor, or Issuer Enrollment Assister.
It is up to you to choose someone to help you if you want or need that help. Neither MassHealth nor the Massachusetts Health Connector will choose or assign a person for you.
About Certified Enrollment Assisters
Enrollment Assisters are people who can help you with your application and enrollment in coverage. They can help you understand new coverage options available as a result of national health care reform and find the most affordable coverage that meets your needs. Enrollment Assisters can be Navigators, Certified Application Counselors, Issuer Enrollment Assisters, or Authorized Representatives.
Authorized Representatives
If you get help from another type of assister such as a friend, family member, or other person, this person may need to complete an Authorized Representative Designation (ARD) Form (or sufficiently similar document), and mail or fax the form to MassHealth. In addition to providing your authorized representative’s information on the “Who’s helping you?” screen, an Authorized Representative Designation form should be completed for certain situations:
- If because of a mental or physical condition, you cannot designate an authorized representative in writing, a person (not an organization) who is acting responsibly on your behalf can be your authorized representative if that person certifies, by filling out an ARD Form, that you are not able to provide a written designation, and that he or she is acting responsibly on your behalf.
- An authorized representative can also be someone who has been appointed by law to act on your behalf. This person must fill out the ARD Form and either you or this person must submit to us, together with this form, a copy of the applicable legal document stating that this person is lawfully representing you.
- A person appointed by law to act on behalf of the estate of an applicant or member who has died can also serve as an authorized representative by following the instructions in the ARD Form. An authorized representative may be a legal guardian, conservator, holder of power of attorney, or health care proxy, or, if the applicant or member has died, the estate’s administrator or executor. What this person is authorized to do for you or for the applicant or member’s estate will depend on the wording of the legal appointment.You must provide the authorized representative’s date of birth and an e-mail address, if he or she has one, so that we can prove his or her identity and protect your privacy
NOTE: An authorized representative has the authority to act on an applicant’s or member’s behalf in all matters with MassHealth and the Health Connector, and will receive personal information about the applicant or member until we receive a cancellation notice terminating their authority. Their authority will not automatically terminate once we process your application.
ID proofing is one of the first steps of the process to apply for health coverage through the Health Connector website. ID proofing is a requirement of the Affordable Care Act (ACA) and must be completed in order for you to submit an application through the Health Connector website. ID proofing is used to verify your identity and is done by asking you questions based on your personal and financial history.
Will ID Proofing affect my credit report or credit score?
When you check credit report after ID Proofing, you may see an inquiry from the Centers for Medicare & Medicaid Services, or CMS. CMS uses credit reporting agencies like Experian to verify the information on your eligibility application. This is only an inquiry and does not affect your credit score. Your eligibility application and credit score will not be affected by the inquiries from Experian or CMS.
Why do I need to verify my identity?
To protect your personal information, you have to take a few steps to verify your identity before you can complete an application. First you will provide information when you create your profile. This information will be used for the first step of ID proofing. Once your information is verified, the ID proofing process will ask you questions that only you would be likely to know the answers to, based on your financial accounts and personal information in your credit report. This process is meant to prevent an unauthorized person from creating an account and applying for health coverage in your name without your knowledge.
What information will I need to verify my identity?
You should be prepared to provide accurate answers to questions about your personal and financial history. You will not be asked about all of these issues, but having this information handy will be helpful:
- Addresses of current and past residences
- Names of counties resided in, past and present
- Auto ownership—Details of the car, the license plate, and any auto loans
- Names of current and previous employers
- Credit cards—Name of lenders, year and month the account was opened
- Mortgages—Name of the lenders, amount of mortgage, and the term (the number of months or years) of the loan
- Loans (including Auto, Student, and Home Equity Loans)—including the name of the lender, amount of loan, and term (the number of months or years) of the loan
About 90% of people that apply through the Health Connector pass ID proofing. You will have 3 chances to enter your information in order to pass. If you do not pass the first time, you can try adding a middle name, suffix, or Social Security number, if you have these, to improve your chances of passing the first step of ID proofing.
What does it mean when the Health Connector tells me that my identity couldn’t be verified?
If you get a message on the Health Connector site that tells you that your identity couldn’t be verified, it simply means that we couldn’t match all of the information you provided with the information available in the electronic records we use for verification. It does not mean that we will not be able to verify your identify, but that we need to take some additional steps to do so.
Some reasons why you may not be able to pass ID proofing is if you have moved within the last year or you have a locked credit report. Sometimes, adding some additional information about yourself, like a middle name, suffix, or Social Security number.
If the Health Connector website tells me that my identity couldn’t be verified, what is the next step?
If the Health Connector website informs you that your identity couldn’t be verified online, you’ll need to send proper documentation—such as a copy of your driver’s license; U.S. passport; or another identification card issued by the federal, state, or local government (for example a Massachusetts State ID card)—in order to continue your application. See the full list below:
ID Proofing Accepted Documents
- Driver’s license issued by state or territory
- School identification card
- Voter Identification card
- military draft card or draft record
- Identification card issued by the federal, state, or local government
- U.S. passport or U.S. passport card
- Certificate of Naturalization (Form N-550 or N-570) or Certificate of U.S. Citizenship (Form N-560 or N-561)
- Permanent Resident Card or Alien Registration Receipt Card (Form I-551)
- Employment Authorization Document that contains a photograph (Form I-766)
- Military dependent’s identification card
- Native American Tribal document
- Coast Guard Merchant Mariner card
- Foreign passport, or identification card issued by a foreign embassy or consulate that contains a photograph
If you can’t provide a copy of one of the above documents, you can send us a copy of two of the following documents instead:
- Birth certificate
- Social Security card
- Marriage certificate
- Divorce decree
- Employer identification card
- High school or college diploma (including high school equivalency diplomas)
- Property deed or title
You can send us documents in the following ways:
- Fax: 617-887-8745
- Mail:
Health Connector
133 Portland Street 1st floor
Boston, MA 02114-1707 - Walk-In: Call Customer Service at 1-877-MA ENROLL (1-877-623-6765) if you would like to bring your documents to one of our walk-in centers:
Boston
Massachusetts Health Connector
133 Portland Street, 1st Floor
Boston, MA 02114-1707
Worcester
Massachusetts Health Connector
146 Main Street, Suite 201/202
Worcester, MA 01608
Please don’t send original documents. The document(s) you send must have either a photograph or other identifying information such as name, age, sex, race, height, weight, eye color, or address. We may ask you additional questions about your documentation in order to verify your identity.
After your documentation is received and processed, you will receive a phone call and/or email to let you know that either your identity was verified or further information is still required.
Note—The Health Connector and MassHealth are required to abide by strict privacy and security standards to make sure your information is protected.
What if I have sent in documents but I have not yet received a notice informing me that my identity verification has been processed?
Please contact the Health Connector or MassHealth Customer Service Center to check for a status update:
- Health Connector:1-877-MA-ENROLL (1-877-623-6765), or TTY 711 for people who are deaf, hard of hearing, or speech disabled.
- MassHealth: 1-800-841-2900, or TTY 1-800-497-4648 for people who are deaf, hard of hearing, or speech disabled.
I continue to have issues verifying my identity, how can I apply for coverage?
If, after you submitted your verification documents and received confirmation that you can continue with your application, but continue to have issues verifying your identity you can:
- Call the Health Connector or MassHealth Customer Service Center to help you complete your application, or
- Mail in a paper application to Health Connector Processing Center, P.O. Box 4404, Taunton, MA 02780 or fax to 617-887-8770.
What if I already submitted a paper application or I applied through the Customer Service Center and I received a notice with my eligibility determination, but now I am having difficulty creating an online account to enroll in coverage?
Don’t worry! Your eligibility determination will be maintained until you are able to select and enroll in a plan, as long as you do so before the end of the enrollment period. Please follow the steps above in order for the Health Connector to verify your identity.You can also call Health Connector Customer Service for help with selecting and enrolling in a plan at 1-877-MA-ENROLL (1-877-623-6765), or TTY 711 for people who are deaf, hard of hearing, or speech disabled.
Content Adapted from “FAQ on Remote Identity Proofing, Remote Identity Proofing Failures and Application Inconsistencies (Federally-facilitated Marketplace)”, last updated May 21, 2014. https://marketplace.cms.gov/technical-assistance-resources/remote-identity-proofing-faqs.pdf
Because of this requirement, when you complete your application, and have dependents listed, the system will ask you how you are related to each dependent more than once. As a result, completing this section of the application may be a little confusing. These questions cannot be skipped in order to get an accurate eligibility determination. Please read all the options carefully before answering these questions and ensure you double-check your work before submitting your application.
Income sources to include:
For each of the following sources, make your best estimate for what your income will be in 2025.
- Wages
- Salaries
- Tips
- Net income from any self-employment or business
- Unemployment compensation
- Social Security payments, including disability payments
- Alimony
- Any other taxable income such as retirement income, investment income, pension income, rental income, prizes, awards, and gambling winnings
Do NOT include the following as income:
- Child support
- Gifts
- Supplemental Security Income (SSI)
- Veterans’ disability payments
- Workers’ compensation
- Proceeds from loans (such as student loans, home equity loans, or bank loans)
Do NOT include any money that an employer takes out of your paycheck such as:
- Child care
- Health insurance
- Retirement plans
These “not taxable” items should be listed explicitly on your paycheck.
Please be sure to double-check that the information you have entered is correct. There is a summary page at the end of the Income section of the application where you can review your information. Take care to note that the income amount has the appropriate yearly/monthly/or weekly label.
“Minimum Value” standards mean that the health plan will pay at least 60% of the total cost of medical services for a standard population. The other 40% of costs would be paid by members through deductibles, co-pays, and co-insurance. Most employer plans meet the Minimum Value standards. To find out for sure if your employer’s plan meets these standards, talk to your human resources department or the health plan. You can use the worksheet we developed to collect their answers. Download the worksheet by clicking here.
How do I know if my employer’s plan is affordable?
If you need help understanding your rights and responsibilities, you can get help from a customer service representative or an Enrollment Assister.
Incarcerated household members
Because of Affordable Care Act (ACA) and Medicaid rules, people who are in jail because they have been convicted of a crime are not eligible to get coverage through the Marketplace.
However, if someone in your household is in jail awaiting trial (pending disposition), that person is still eligible to apply for coverage through the Health Connector website.
When you apply, you will be asked on the “Rights and Responsibilities” page if someone applying for coverage is incarcerated. Only respond “Yes” if there is a person who is applying with you and they are in jail because they were convicted of a crime (not awaiting disposition).
e-Signature
Your Electronic Signature—or e-Signature—allows you sign documents online.
If you are having trouble with the e-Signature, such as getting an error message—for example, “Your e-Signature does not match the Head of Household’s name. Please note that this field is case-sensitive”—first, check and make sure that the name you typed into the e-Signature box is exactly how you typed it when you created an account. If it looks right, then check to make sure you did not accidentally include any extra spaces or punctuation.
EXAMPLE:
How you entered your name on your account information:
John S Doe Jr.
How you should enter your e-Signature:
| Correct | Not Correct |
| John S Doe | John S Do e (contains an extra space)John DOE (case does not match)John S. Doe (do not include a period after your middle initial) |
| John Doe | John S Doe, Jr. (do not include a suffix or extra punctuation) |
Other tips:
- If you entered a middle initial when you created your account, you may not need to include it in your e-Signature. If you do enter your middle initial and get an error message, try entering your signature without it.
- Do not use a period after your middle initial.
- Do not include your suffix (like Jr., Sr., etc.) that you selected when you created your account.
- If you accidentally put an extra space in your name when you created your account, this may cause errors because your signature must match exactly.
- Alien number: The alien number (also called alien registration number or USCIS number) can be found on the immigration document. It starts with an “A” and ends with 8 or 9 numbers. If your card has 8 numbers enter the A before the 8 numbers, if your card has 9 numbers please enter just the 9 numbers. If you also have a card number, you should enter both, if possible. If you have a card number, but don’t enter it, it will take longer to verify your status.
- Card number: The card number can be found on several immigration documents, including the I-766 Employment Authorization Card and the I-551 Lawful Permanent Resident Card. A card number starts with 3 letters and ends with 10 numbers. If you also have an alien number or if other document information is requested, you should enter all, if possible. If you have a card number, but don’t enter it, it will take longer to verify your status.
- I-94 number: The I-94 number (also called the admission number) is printed on the I-94 or I-94A. This is an 11-digit number and is usually found at the top, left-hand side of the document. Note: In some cases, Customs and Border Protection may have struck out the pre-printed I-94 number and hand-written a different number on the form. If this is the case, enter the hand-written number.
- Passport number: The passport number can be found on the passport. It can be 6 to 12 numbers long.
- Country of issuance: Select the country which issued the passport.
- Passport expiration date: Enter the date the passport will expire (month, day, year). The expiration date should be listed on the document.
- SEVIS ID number: The SEVIS ID (Form I-20 or DS2019) which is 10 numbers long and is located at the top, right-hand corner of the document.
- Document expiration date: Enter the expiration date (month, day, year) listed on the document.
- Category code: Enter the 3-digit code listed on the employment authorization document. This code starts with an “A,” “B,” or “C.”
If you have trouble finding information on your document or you’re getting errors when trying to submit your application, answer “Yes” if you have eligible immigration status when asked this question, then continue your application without entering your document numbers. If you don’t enter your document information, you may be asked to provide a copy of your document after you submit your application.
Eligibility Results
People can use this website to apply for MassHealth coverage, the Children’s Medical Security Plan and the Health Safety Net. People who qualify for MassHealth coverage after completing the online application cannot shop for Health Connector or ConnectorCare plans.
If you or some of your household members have been approved for coverage through MassHealth, those people will get a letter from MassHealth in 3–5 business days with more information about their coverage and health plan options available. If you have any questions, you can visit the MassHealth website and find out more in the Member Booklet for Health Coverage and Help Paying Costs or contact MassHealth Customer Service at 1-800-841-2900, or TTY 1-800-497-4648 for people who are deaf, hard of hearing, or speech disabled.
After you complete your eligibility application, you may see that you need to send in verification documents, or proof, of information you have submitted. After you submit your application online, you will see an eligibility determination page that shows the programs your household qualifies for, as well as the type of document that you will need to send to the Health Connector as proof. You will also see a list of the different kinds of documents that count as acceptable proof.
In addition to this list available online, each household member will receive a letter in the mail requesting the same verification materials. Depending on which coverage people in your household qualify for, they may receive notices from both the Health Connector and MassHealth requesting the same information. These notices are valid and you will need to respond to each notice in order to complete your application and/or enrollment process.
You can learn more about the types of proof that may be required on our Verification Document information page.
Example detail of a Dashboard page with a sample list of “Documents you need to provide”

Sample Notice Requesting Verification Documents
Tip: You can still enroll in Health Connector and ConnectorCare plans while verifications (proof) are being processed, which can take up to 90 days. If you are eligible for MassHealth and need to send proof of income, you will need to do so before you can complete your enrollment. You will get a letter from either MassHealth or the Health Connector with any next steps you need to take within 30 days of completing your online application. This may take longer if you completed a paper application.
Shopping for Plans
- Your monthly plan premium
- Your plan’s deductible
- Your maximum out-of-pocket costs
- What prescription drugs are covered and how much you will pay
- What is covered and how much you will pay if you see a doctor or go to the emergency room
- If your provider, or doctor, accepts the plan
You can find this information on each plan’s Summary of Benefits and Coverage (SBC). This is where you can find the most comprehensive information on any plan. To see a plan’s SBC while you are browsing for plans, go to the plan detail page. At the bottom of the page are links to Plan Documents. You can find SBCs there.
Additionally, when you are selecting a plan, it is very important that you check that your doctor is in that plan’s network (a network is the group of providers that participate with a certain health plan). You will find links to health plan websites on the Health Connector website. Be sure to visit the “find a doctor” tool (Provider Search) on these websites before enrolling in a plan to ensure that your doctor will be available to you.
If you want to purchase a stand-alone dental plan without purchasing a health plan, please follow these steps:
- Complete an online eligibility application
- Anonymously preview dental plans and determine which plan you would like to purchase from available options
- Once you have identified a plan, contact Health Connector customer service to purchase your stand-alone dental plan over the phone. Call 1-877-MA-ENROLL (1-877-623-6765), or TTY 711 for people who are deaf, hard of hearing, or speech disabled.
If you are eligible to shop for catastrophic plans and intend to enroll in one, you can either:
- Complete an application for insurance without help paying for costs to shop for these plans online. To do so, answer “no” to the question, “Are you seeking financial assistance?” when you complete your application.
or
- You may need to contact Health Connector customer service in order to purchase a catastrophic health plan over the phone. Call 1-877-MA-ENROLL (1-877-623-6765), or TTY 711 for people who are deaf, hard of hearing, or speech disabled.
Please remember to carefully review Summaries of Benefits and Coverage for this plan type to ensure the coverage meets your needs. If you are not sure, you can contact a local Enrollment Assister to help you understand your coverage options.
To change your APTC amount, while you are shopping for plans:
- Click the “Change Tax Credit” link in the top paragraph of the page that explains what the Advance Premium Tax Credit is and how much you are eligible for.
- When you click the link, it will open a modal window that includes a slider to increase or lower the amount of tax credit you want to apply to your monthly premium.
- Then, click “Save” to save your changes.
Enrollment
For example, if you sign up for a plan that starts January 1, 2025, then you must make your first premium payment by December 23, 2024.
Please note you will not be enrolled in your health or dental plan until you pay the first month’s premium in full by the due date.
Once you make your first payment, it will take about five business days before your insurance carrier will be able to confirm your enrollment. Once your enrollment is confirmed, you will receive a Welcome Letter from the Health Connector. Your insurance carrier will send you an ID card within approximately 2 weeks after the Health Connector receives your full payment.
Monthly Plan Selection and Payment Deadlines
| Payment Due Date | Coverage Start Date |
|---|---|
| December 23, 2024 | January 1, 2025 |
| January 23, 2025 | February 1, 2025 |
| February 23, 2025 | March 1, 2025 |
| March 23, 2025 | April 1, 2025 |
| April 23, 2025 | May 1, 2025 |
| May 23, 2025 | June 1, 2025 |
| June 23, 2025 | July 1, 2025 |
| July 23, 2025 | August 1, 2025 |
| August 23, 2025 | September 1, 2025 |
| September 23, 2025 | October 1, 2025 |
| October 23, 2025 | November 1, 2025 |
| November 23, 2025 | December 1, 2025 |
| December 23, 2025 | January 1, 2026 |






